About Q Fever
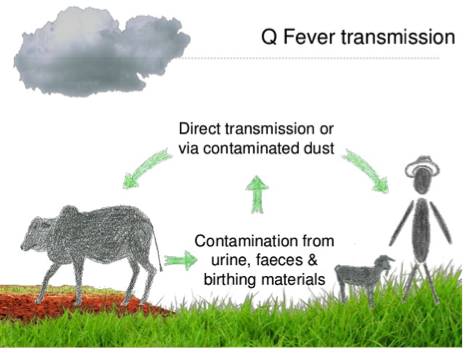
Q Fever is an infection that produces flu-like symptoms in humans but can progress to more serious symptoms and chronic illness in some cases. It is spread to humans from infected livestock and wildlife, although animals rarely show symptoms. It is most commonly transmitted by inhaling infected dust and contaminated droplets containing the bacterium – Coxiella burnetii. The bacterium is highly contagious within herds of domestic cattle, sheep, goats, and wild pigs.
The bacterium is found in infected animals’ urine, faeces, birth fluids, the placenta of a foetus or newborn as well as in uterine discharges following birth. These materials will contain high concentrations of the bacterium.
The organism is highly contagious within domestic herds and will spread quickly through stock. Once a herd is infected it will almost invariably spread to neighbouring stock, native and feral animals, and sometimes domestic cats and dogs. Once a herd is infected, it normally remains infected.
Direct or indirect inhalation of the bacterium is the most common mechanism of human infection. However, the human infection can also occur via skin abrasions and splashes of infected material into the eye. The consumption of unpasteurised milk from infected cows and goats has accounted for small numbers of Q Fever cases.
The Coxiella burnetii bacterium is resistant to heat, drying and many common disinfectants, allowing it to survive for lengthy periods in the environment. Infection can also be transmitted by direct contact with objects (boots, clothing) and ingestion (for example eating after you’ve handled animals and not washing your hands).
Usually, Q Fever is an occupational disease of meat workers, farmers, and veterinarians. People who hunt and slaughter wild goats and pigs are also at risk. However, living in a regional or remote area puts you at high risk even if you don’t work with animals.
Signs and symptoms of Q Fever
- Fever, which may last for up to four weeks.
- Severe headache, blurred vision or light sensitivity.
- Sweats and chills.
- Tiredness – prolonged fatigue may follow infection (post Q Fever fatigue syndrome).
- Muscle aches.
- Confusion.
- Sore throat.
- Dry cough.
- Chest pain on breathing.
- Nausea, vomiting and diarrhoea.
- Weight loss.
- Abdominal pain
Diagnosis of Q Fever is made via a series of blood tests. Effective treatment includes antibiotic therapy. With early diagnosis, treatment is simple, and a good outcome can be expected.
The use of personal protective equipment (gloves, P2 dust mask and waterproof overalls) will minimise your risk of exposure to infected body materials or inhalation of infected particles in the air. The most effective prevention strategy is immunisation against the disease and is achieved through vaccination with the Q Fever vaccine (Q –Vax). This can be given to at-risk people who are aged 15 years and over.
Steps towards identifying, developing and registering Q Fever immunity
Initial – blood and a skin test
This is recommended to ascertain if the individual has previously been exposed to Q Fever – either naturally or by previous vaccination. In many cases, people have been unknowingly infected previously with a mild strain of the disease, which was not confirmed by a doctor as Q Fever.
Interpretations – blood test and skin test
If interpretation confirms as – previously being infected with the disease, vaccination is unnecessary.
Implementation – Q-vax vaccination (if no immunity identified)
Once vaccinated, the vaccine will be recorded on the Australian Immunisation Register (AIR). People with an existing record with the Q Fever Register can access their information until 30/6/2025 at qfever.org. You may download your existing eStatement and have the details reported to the Australian Immunisation Register by a recognised vaccination provider.
Contact your local GP or state health listed Q Fever provider for testing and vaccination services.
Find out more information on Q Fever visit Better Health Channel.
Fast facts:
- Q Fever is spread to humans from cattle, sheep, goats and wild pigs.
- People can become infected when splashed with infected body fluids or by breathing infected dust.
- Q Fever causes flu like symptoms and can be dangerous for people with heart problems.
- Wear protective clothing and consider vaccination if you are at risk of infection.
References used for this topic
More information:
US Centers for Disease Control and Prevention
Clinical care:
Department of Health Australia
Information about Q Fever disease, vaccines and recommendations for vaccination from the Australian Immunisation Handbook
Royal College of Pathologists of Australia Manual
Q Fever
SA Health
Q Fever – including symptoms, treatment and prevention
Victorian Department of Health
Q Fever
Research & reviews:
Open Veterinary Journal
Navigating Q Fever: Current perspectives and challenges in outbreak preparedness – PMC (nih.gov)
International Journal of Microbiology
Q Fever: Current State of Knowledge and Perspectives of Research of a Neglected Zoonosis
Australian Journal of Pharmacy
Q Fever and Australian farmers: is the health system paying enough attention? A literature review
Medical Journal of Australia
Seroprevalence of Q Fever among metropolitan and non‐metropolitan blood donors in New South Wales and Queensland, 2014–2015
AgriFutures Australia
|
|